|
|
|
| Miniaturization in percutaneous nephrolithotomy: What is new? |
Wei Zhu,Zhicong Huang,Guohua Zeng( ) )
|
| Department of Urology and Guangdong Key Laboratory of Urology, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China |
|
|
|
|
Abstract Objective To summarize recent advancements in mini-percutaneous nephrolithotomy (mini-PCNL) in surgical technique, stone removal strategy, lithotripsy, and surgical model from the current literature.
Methods We conducted a narrative review of relevant English-language articles up to October 2022 using the PubMed and Web of Science databases. The following keywords were used in the search: “percutaneous nephrolithotomy”, “minimally invasive percutaneous nephrolithotomy”, “mini-PCNL”, “mini-perc”, “mPCNL”, and “miniaturization”.
Results A series of new progress has been made in many aspects of mini-PCNL, such as further reduction of tract size—needle perc and further improvement of robotic-assisted PCNL—artificial intelligence-powered robotic devices.
Conclusion Many studies and trials have been conducted to reduce morbidity and increase the safety and effectiveness of mini-PCNL. It is crucial to realize that miniaturization of PCNL requires not only a smaller percutaneous tract size, but also an adjustment strategically in renal access, stone removal, lithotripsy, and surgical model in general. More large-scale prospective research needs to be carried out to further validate and optimize the safety and effectiveness of mini-PCNL.
|
|
Received: 16 October 2022
Available online:
|
|
Corresponding Authors:
Guohua Zeng
E-mail: gzgyzgh@vip.sina.com
|
|
|
| Term | Access sheath, Fr | Reference | | Mini-PCNL | ≤22 | Jackman et al. [1] | | Minimally invasive PCNL | 9.5-26 | Nagele et al. [9] | | Chinese minimally invasive PCNL | 14-20 | Zeng et al. [8] | | Ultra-mini PCNL | 11-13 | Desai and Solanki [10] | | Super-mini PCNL | 10-14 | Zeng et al. [12] | | Micro-PCNL | 4.8 | Desai and Mishra [11] | | Needle-perc | 4.2 | Xiao et al. [7] |
|
|
Current nomenclature of mini-PCNL techniques.
|

|
|
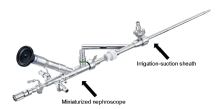
4.2 Fr needle-perc [7].
|
|
|
Super-mini percutaneous nephrolithotomy system [12,13].
|
| [1] |
Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: experience with a new technique. Urology 1998; 52:697-701.
doi: 10.1016/s0090-4295(98)00315-x
pmid: 9763096
|
| [2] |
Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The “mini-perc” technique: a less invasive alternative to percutaneous nephrolithotomy. World J Urol 1998; 16:371-4.
doi: 10.1007/s003450050083
pmid: 9870281
|
| [3] |
Lahme S, Bichler KH, Strohmaier WL, G?tz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol 2001; 40:619-24.
doi: 10.1159/000049847
pmid: 11805407
|
| [4] |
Choong S, de la Rosette J, Denstedt J, Zeng G, Sarica K, Mazzon G, et al. Classification and standardized reporting of percutaneous nephrolithotomy (PCNL): International Alliance of Urolithiasis (IAU) consensus statements. Minerva Urol Nephrol 2022; 74:110-8.
doi: 10.23736/S2724-6051.20.04107-7
pmid: 33439573
|
| [5] |
Tepeler A, Sarica K. Standard, mini, ultra-mini, and micro percutaneous nephrolithotomy: what is next? A novel labeling system for percutaneous nephrolithotomy according to the size of the access sheath used during procedure. Urolithiasis 2013; 41:367-8.
doi: 10.1007/s00240-013-0578-3
pmid: 23736743
|
| [6] |
Wright AE, Somani BK, Rukin NJ. Proposition for new terminologies in PCNL: what does “ultra-mini-micro” actually mean? Urolithiasis 2014; 42:539-40.
doi: 10.1007/s00240-014-0696-6
pmid: 25085200
|
| [7] |
Xiao B, Ji CY, Su BX, Hu WG, Fu M, Li JX. Needle-perc: a new instrument and its initial clinical application. Chin Med J 2020; 133:732-4.
|
| [8] |
Zeng G, Zhao Z, Wan S, Mai Z, Wu W, Zhong W, et al. Minimally invasive percutaneous nephrolithotomy for simple and complex renal caliceal stones: a comparative analysis of more than 10 000 cases. J Endourol 2013; 27:1203-8.
|
| [9] |
Nagele U, Horstmann M, Sievert KD, Kuczyk MA, Walcher U, Hennenlotter J, et al. A newly designed amplatz sheath decreases intrapelvic irrigation pressure during minipercutaneous nephrolitholapaxy: an in-vitro pressure-measurement and microscopic study. J Endourol 2007; 21: 1113-6.
pmid: 17941796
|
| [10] |
Desai J, Solanki R. Ultra-mini percutaneous nephrolithotomy (UMP): one more armamentarium. BJU Int 2013; 112:1046-9.
doi: 10.1111/bju.12193
pmid: 23841665
|
| [11] |
Desai M, Mishra S. ‘Microperc’ micro percutaneous nephrolithotomy: evidence to practice. Curr Opin Urol 2012; 22: 134-8.
doi: 10.1097/MOU.0b013e32834fc3bb
|
| [12] |
Zeng G, Wan S, Zhao Z, Zhu J, Tuerxun A, Song C, et al. Supermini percutaneous nephrolithotomy (SMP): a new concept in technique and instrumentation. BJU Int 2016; 117:655-61.
doi: 10.1111/bju.13242
|
| [13] |
Zeng G, Zhu W, Liu Y, Fan J, Zhao Z, Cai C. The new generation super-mini percutaneous nephrolithotomy (SMP) system: a step-by-step guide. BJU Int 2017; 120:735-8.
doi: 10.1111/bju.13955
pmid: 28692204
|
| [14] |
Cheng F, Yu W, Zhang X, Yang S, Xia Y, Ruan Y. Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol 2010; 24:1579-82.
doi: 10.1089/end.2009.0581
pmid: 20839954
|
| [15] |
Abdelhafez MF, Bedke J, Amend B, ElGanainy E, Aboulella H, Elakkad M, et al. Minimally invasive percutaneous nephrolitholapaxy (PCNL) as an effective and safe procedure for large renal stones. BJU Int 2012; 110:E1022-6. https://doi.org/10.1111/j.1464-410X.2012.11191.x.
doi: 10.1111/bju.2012.110.issue-11c
|
| [16] |
Xiao B, Diao X, Jin S, Ji C, Zhang G, Su B, et al. A novel surgical technique for treatment of renal stones in preschool-aged patients: initial experience with needle-perc. Urology 2020; 146:211-5.
doi: 10.1016/j.urology.2020.07.055
pmid: 32791292
|
| [17] |
Zhu W, Li J, Yuan J, Liu Y, Wan SP, Liu G, et al. A prospective and randomised trial comparing fluoroscopic, total ultrasonographic, and combined guidance for renal access in minipercutaneous nephrolithotomy. BJU Int 2017; 119:612-8.
doi: 10.1111/bju.2017.119.issue-4
|
| [18] |
Su LM, Stoianovici D, Jarrett TW, Patriciu A, Roberts WW, Cadeddu JA, et al. Robotic percutaneous access to the kidney: comparison with standard manual access. J Endourol 2002; 16: 471-5.
doi: 10.1089/089277902760367421
|
| [19] |
Oo MM, Gandhi HR, Chong KT, Goh JQ, Ng KW, Hein AT, et al. Automated needle targeting with X-ray (ANT-X)-robot-assisted device for percutaneous nephrolithotomy (PCNL) with its first successful use in human. J Endourol 2021; 35:e919. https://doi.org/10.1089/end.2018.0003.
doi: 10.1089/end.2018.0003
|
| [20] |
Taguchi K, Hamamoto S, Okada A, Sugino T, Unno R, Kato T, et al. A randomized, single-blind clinical trial comparing robotic-assisted fluoroscopic-guided with ultrasound-guided renal access for percutaneous nephrolithotomy. J Urol 2022; 208:684-94.
doi: 10.1097/JU.0000000000002749
|
| [21] |
Zhong W, Wen J, Peng L, Zeng G. Enhanced super-mini-PCNL (eSMP): low renal pelvic pressure and high stone removal efficiency in a prospective randomized controlled trial. World J Urol 2021; 39:929-34.
doi: 10.1007/s00345-020-03263-3
|
| [22] |
Du C, Song L, Wu X, Fan D, Zhu L, Liu S, et al. Suctioning minimally invasive percutaneous nephrolithotomy with a patented system is effective to treat renal staghorn calculi: a prospective multicenter study. Urol Int 2018; 101:143-9.
doi: 10.1159/000488399
pmid: 29649833
|
| [23] |
Zhu Z, Cui Y, Zeng H, Li Y, He C, Chen J, et al. Suctioning versus traditional minimally invasive percutaneous nephrolithotomy to treat renal staghorn calculi: a case-matched comparative study. Int J Surg Lond Engl 2019; 72:85-90.
|
| [24] |
Sarica K, Eryildirim B, Tuerxun A, Batuer A, Kavukoglu O, Buz A, et al. Super-mini percutaneous nephrolithotomy for renal stone less than 25 mm in pediatric patients: could it be an alternative to shockwave lithotripsy? Actas Urol Esp 2018; 42:406-13.
doi: 10.1016/j.acuro.2017.08.005
|
| [25] |
Alken P. Is supermini-percutaneous nephrolithotomy a new way forward? BJU Int 2020; 125:483-4.
|
| [26] |
Liu Y, Cai C, Aquino A, Al-Mousawi S, Zhang X, Choong SKS, et al. Management of large renal stones with super-mini percutaneous nephrolithotomy: an international multicentre comparative study. BJU Int 2020; 126:168-76.
doi: 10.1111/bju.15066
pmid: 32279423
|
| [27] |
Zhong W, Zeng G, Wu W, Chen W, Wu K. Minimally invasive percutaneous nephrolithotomy with multiple mini tracts in a single session in treating staghorn calculi. Urol Res 2011; 39: 117-22.
doi: 10.1007/s00240-010-0308-z
pmid: 20821200
|
| [28] |
Giusti G, Piccinelli A, Taverna G, Benetti A, Pasini L, Corinti M, et al. Miniperc? No thank you. Eur Urol 2007; 51:810-5.
doi: 10.1016/j.eururo.2006.07.047
pmid: 16938385
|
| [29] |
Patil A, Reddy N, Shah D, Singh A, Ganpule A, Sabnis R, et al. High-power holmium with Moses technology or thulium fiber laser in MiniPerc with suction: a new curiosity. J Endourol 2022; 36:1348-54.
doi: 10.1089/end.2021.0915
|
| [30] |
Shah D, Patil A, Reddy N, Singh A, Ganpule A, Sabnis R, et al. A clinical experience of thulium fibre laser in miniperc to dust with suction: a new horizon. World J Urol 2021; 39:2727-32.
doi: 10.1007/s00345-020-03458-8
pmid: 32960327
|
| [31] |
Elhilali MM, Badaan S, Ibrahim A, Andonian S. Use of the Moses technology to improve holmium laser lithotripsy outcomes: a preclinical study. J Endourol 2017; 31:598-604.
doi: 10.1089/end.2017.0050
pmid: 28340540
|
| [32] |
Aldoukhi AH, Roberts WW, Hall TL, Ghani KR. Holmium laser lithotripsy in the new stone age: dust or bust? Front Surg 2017; 4:57. https://doi.org/10.3389/fsurg.2017.00057.
doi: 10.3389/fsurg.2017.00057
pmid: 29067287
|
| [33] |
Blackmon RL, Irby PB, Fried NM. Comparison of holmium:YAG and thulium fiber laser lithotripsy: ablation thresholds, ablation rates, and retropulsion effects. J Biomed Opt 2011; 16: 071403. https://doi.org/10.1117/1.3564884.
doi: 10.1117/1.3564884
|
| [34] |
Traxer O, Keller EX. Thulium fiber laser: the new player for kidney stone treatment? A comparison with holmium:YAG laser. World J Urol 2020; 38:1883-94.
doi: 10.1007/s00345-019-02654-5
pmid: 30729311
|
| [35] |
De CV, Keller EX, Kovalenko A, Vinnichenko V, Traxer O. Mp03-20 dusting efficiency comparison between moses technology of Ho:YAG laser and superpulse thulium fiber laser. J Urol 2019; 201:e28-9. https://doi.org/10.1097/01.JU.0000554952.38129.59.
|
| [36] |
Kronenberg P, Traxer O. The laser of the future: reality and expectations about the new thulium fiber laserda systematic review. Transl Androl Urol 2019; 8:S398-417. https://doi.org/10.21037/tau.2019.08.01.
doi: 10.21037/tau.2019.08.01
|
| [37] |
Zeng G, Cai C, Duan X, Xu X, Mao H, Li X, et al. Mini percutaneous nephrolithotomy is a noninferior modality to standard percutaneous nephrolithotomy for the management of 20-40 mm renal calculi: a multicenter randomized controlled trial. Eur Urol 2021; 79:114-21.
|
| [38] |
Zhu W, Liu Y, Liu L, Lei M, Yuan J, Wan SP, et al. Minimally invasive versus standard percutaneous nephrolithotomy: a meta-analysis. Urolithiasis 2015; 43:563-70.
doi: 10.1007/s00240-015-0808-y
pmid: 26242465
|
| [39] |
Wu X, Zhao Z, Sun H, Cai C, Li Z, Cheng D, et al. Day-surgery percutaneous nephrolithotomy: a high-volume center retrospective experience. World J Urol 2020; 38:1323-8.
doi: 10.1007/s00345-019-02942-0
pmid: 31522237
|
| [40] |
Zhao Z, Sun H, Wu X, Cai C, Liu Y, Zeng G. Evaluation of daycare versus inpatient mini-percutaneous nephrolithotomy: a propensity score-matching study. Urolithiasis 2020; 48: 209-15.
doi: 10.1007/s00240-019-01160-y
|
| [41] |
Zhu H, Zhao Z, Cheng D, Wu X, Yue G, Lei Y, et al. Multipletract percutaneous nephrolithotomy as a day surgery for the treatment of complex renal stones: an initial experience. World J Urol 2021; 39:921-7.
doi: 10.1007/s00345-020-03260-6
|
| [42] |
Jones P, Bennett G, Dosis A, Pietropaolo A, Geraghty R, Aboumarzouk O, et al. Safety and efficacy of day-case percutaneous nephrolithotomy: a systematic review from European Society of Uro-technology. Eur Urol Focus 2019; 5: 1127-34.
doi: S2405-4569(18)30091-9
pmid: 29657068
|
| [43] |
Zhao Z, Yin S, Zhu H, Cheng D, Liu Y, Zeng G. The feasibility of multiple-tract mini-percutaneous nephrolithotomy as an overnight surgery for the treatment of complex kidney stones. Urolithiasis 2021; 49:167-72.
doi: 10.1007/s00240-020-01208-4
|
| [44] |
Cracco CM, Scoffone CM. Endoscopic combined intrarenal surgery (ECIRS)dtips and tricks to improve outcomes: a systematic review. Turk J Urol 2020; 46:S46-57. https://doi.org/10.5152/tud.2020.20282.
|
| [45] |
Widyokirono DR, Kloping YP, Hidayatullah F, Rahman ZA, Ng AC, Hakim L. Endoscopic combined intrarenal surgery vs. percutaneous nephrolithotomy for large and complex renal stone: a systematic review and meta-analysis. J Endourol 2022; 36:865-76.
doi: 10.1089/end.2021.0761
pmid: 35152754
|
| [46] |
Inoue T, Kinoshita H, Okada S, Hamamoto S, Taguchi M, Murota T, et al. Wideband Doppler ultrasound-guided miniendoscopic combined intrarenal surgery as an effective and safe procedure for management of large renal stones: a preliminary report. Urology 2016; 95:60-6.
|
| [47] |
Ong CSH, Biligere S, Mangat R, Thandapani K, Heng CT, Desai M, et al. Micro endoscopic combined intrarenal surgery (microECIRS): a step-by-step guide. Urol Video J 2020; 8:100063. https://doi.org/10.1016/j.urolvj.2020.100063.
|
| [48] |
Jung HD, Kim JC, Ahn HK, Kwon JH, Han K, Han WK, et al. Real-time simultaneous endoscopic combined intrarenal surgery with intermediate-supine position: washout mechanism and transport technique. Investig Clin Urol 2018; 59:348-54. https://doi.org/10.4111/icu.2018.59.5.348.
doi: 10.4111/icu.2018.59.5.348
pmid: 30182081
|
| [1] |
Rasim Güzel,Ümit Yildirim,Kemal Sarica. Contemporary minimal invasive surgical management of stones in children[J]. Asian Journal of Urology, 2023, 10(3): 239-245. |
| [2] |
Giorgio Mazzon,Simon Choong,Antonio Celia. Stone-scoring systems for predicting complications in percutaneous nephrolithotomy: A systematic review of the literature[J]. Asian Journal of Urology, 2023, 10(3): 226-238. |
| [3] |
Qinghui Wu,Kesavan Esuvaranathan,Teck Kheng Lee,Soo Leong Foo,Jian Ping Chai,Edmund Chiong. A pilot clinical study of developing an External Assist Targeting Device for rapid and precise renal calyx access during percutaneous nephrolithotomy[J]. Asian Journal of Urology, 2023, 10(3): 364-371. |
| [4] |
. Reliability of nephrolithometric nomograms in patients treated with minimally invasive percutaneous nephrolithotomy: A precision study[J]. Asian Journal of Urology, 2023, 10(1): 70-80. |
| [5] |
Pankaj N. Maheshwari,Amandeep Arora,Mahesh S. Sane,Vivek Jadhao. Evaluating factors associated with the risk of hydrothorax following standard supracostal percutaneous nephrolithotomy[J]. Asian Journal of Urology, 2022, 9(3): 301-306. |
| [6] |
Sujeet Poudyal. Current insights on haemorrhagic complications in percutaneous nephrolithotomy[J]. Asian Journal of Urology, 2022, 9(1): 81-93. |
| [7] |
Abhishek Gajendra Singh,Sundaram Palaniappan,Shrikant Jai,Gopal Tak,Arvind Ganpule,Ravindra Sabnis,Mahesh Desai. The clinical outcomes of laser with suction device in mini-percutaneous nephrolithotomy[J]. Asian Journal of Urology, 2022, 9(1): 63-68. |
| [8] |
Dilip K. Mishra,Sonia Bhatt,Sundaram Palaniappan,Talamanchi V.K. Reddy,Vinothkumar Rajenthiran,Y.L. Sreeranga,Madhu S. Agrawal. Mini versus ultra-mini percutaneous nephrolithotomy in a paediatric population[J]. Asian Journal of Urology, 2022, 9(1): 75-80. |
| [9] |
Yiwei Wang, Liheng Gao, Mingxi Xu, Wenfeng Li, Yuanshen Mao, Fujun Wang, Lu Wang, Jun Da, Zhong Wang. A novel spherical-headed fascial dilator is feasible for second-stage ultrasound guided percutaneous nephrolithotomy: A pilot study[J]. Asian Journal of Urology, 2021, 8(4): 424-429. |
| [10] |
Sudharsan Balaji,Arvind Ganpule,Thomas Herrmann,Ravindra Sabnis,Mahesh Desai. Contemporary role of multi-tract percutaneous nephrolithotomy in the treatment of complex renal calculi[J]. Asian Journal of Urology, 2020, 7(2): 102-109. |
| [11] |
Etienne Xavier Kellera,Vincent De Conincka,Steeve Doizia,Olivier Traxer. The role of ureteroscopy for treatment of staghorn calculi: A systematic review[J]. Asian Journal of Urology, 2020, 7(2): 110-115. |
| [12] |
Osman Ermis,Bhaskar Somani,Thomas Reeves,Selcuk Guven,Pilar Laguna Pes,Arun Chawla,Padmaraj Hegde,Jean de la Rosette. Definition, treatment and outcome of residual fragments in staghorn stones[J]. Asian Journal of Urology, 2020, 7(2): 116-121. |
| [13] |
Nariman Gadzhiev,Vigen Malkhasyan,Gagik Akopyan,Sergei Petrov,Francis Jefferson,Zhamshid Okhunov. Percutaneous nephrolithotomy for staghorn calculi: Troubleshooting and managing complications[J]. Asian Journal of Urology, 2020, 7(2): 139-148. |
| [14] |
Jared S. Winoker,Ryan A. Chandhoke,William Atallah,Mantu Gupta. Morphometry scores: Clinical implications in the management of staghorn calculi[J]. Asian Journal of Urology, 2020, 7(2): 78-86. |
| [15] |
Arvind P. Ganpule,M. Naveen Kumar Reddy,S.B. Sudharsan,Shaishav B. Shah,Ravindra B. Sabnis,Mahesh R. Desai. Multitract percutaneous nephrolithotomy in staghorn calculus[J]. Asian Journal of Urology, 2020, 7(2): 94-101. |
|
|
|
|