|
|
|
| Prospective randomized study correlating intra-operative urethral mucosal injury with early period after transurethral resection of the prostate stricture urethra: A novel concept |
Suresh B. Patankar,Mayur M. Narkhede*( ),Gururaj Padasalagi,Kashinath Thakare ),Gururaj Padasalagi,Kashinath Thakare
|
| Department of Urology, Ace Hospital, Pune, ASP Medical Foundation, Sripad Medisearch PVT LTD, India |
|
|
|
|
Abstract Objective: To investigate the incidence of urethral stricture during the early period after transurethral resection of the prostate (TURP) and correlate its incidence with intra-operative urethral mucosal injury during TURP. Also to compare the other established risk factors affecting the development of urethral stricture among patients undergoing monopolar or bipolar TURP over a period of 6 months follow-up as the prospective randomized study. Methods: One hundred and fifty men older than 50 years with lower-urinary tract symptoms associated with benign prostatic hyperplasia were randomized to undergo either standard monopolar TURP with glycine as the irrigation fluid or bipolar TURP with normal saline as irrigant. The prostate size, operative time, intra-operative mucosal rupture, catheter time, catheter traction duration, uroflowmetry, and post-operative stricture rate were compared. Results: A total of 150 patients underwent TURP, including 74 patients undergoing monopolar TURP (one patient was excluded as his post-operative histopathological examination report was of adenocarcinoma prostate) and 75 patients undergoing bipolar-TURP, all of which were performed using a 26 Fr sheath resectoscope. The mean International Prostate Symptom Score and maximum urinary flow rate score at post-operative 3 months and 6 months were comparable between the groups. Out of 149 patients, nine patients (6.0%) developed urethral stricture. The severity of the injury (urethral mucosal injury) correlated with the likelihood of developing a subsequent complication (stricture urethra). Patients with stricture had significantly larger prostate volume than patients without stricture (65.0 mL vs. 50.0 mL; p=0.030). Patients with stricture had longer operative time than patients without stricture (55.0 min vs. 40.0 min; p=0.002). In both procedures, formation of post-operative stricture urethra was independently associated with intra-operative mucosal injury. Conclusion: Intra-operative recognition of urethral mucosal injury helps in prediction of stricture urethra formation in early post-operative period.
|
|
Received: 29 May 2023
Available online: 20 July 2024
|
|
Corresponding Authors:
*E-mail address: acehospitalacademics@gmail.com (M.M. Narkhede).
|
|
|
|
|
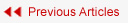
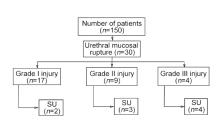
Study flowchart. TURP, transurethral resection of prostate; B-TURP, bipolar TURP; M-TURP, monopolar TURP; PCa, prostate cancer.
|
|
|
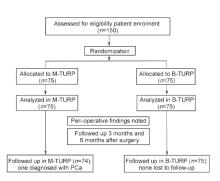
Representative images of urethral mucosal injury. (A and B) Grade I; (C and D) Grade II; (E and F) Grade III.
|
| Parameter | M-TURP (n=74) | B-TURP (n=75) | p-Value | | Prostate size, mL | 57.3±24.9 | 56.0±17.2 | 0.712 | | Prostate size group | | | 0.298 | | <40 mL | 12 (16.2) | 9 (12.0) | | | 40-59 mL | 32 (43.2) | 35 (46.7) | | 60-99 mL | 25 (33.8) | 30 (40.0) | | ≥100 mL | 5 (6.8) | 1 (1.3) | | Comorbiditya | | | - | | Hypertension | 30 (68.2) | 28 (62.2) | | | Diabetes mellitus | 19 (43.2) | 23 (51.1) | | Hypocontractile bladder | 3 (6.8) | 5 (11.1) | | Ischemic heart disease | 2 (4.5) | 2 (4.4) | | Bladder cancer | 1 (2.3) | 1 (2.2) | | Chronic kidney disease | 1 (2.3) | - |
|
|
Demographic characteristics.
|
| Parameter | M-TURP (n=74) | B-TURP (n=75) | p-Value | | Operative time, min | 41.4±12.7 | 40.2±11.2 | 0.523 | | Incidence of urethral mucosa rupture | 15 (20.3) | 15 (20.0) | 0.967 | | Grade of injury | | | | | Grade I | 8 (10.8) | 9 (12.0) | 0.819 | | Grade II | 5 (6.8) | 4 (5.3) | 0.498 | | Grade III | 2 (2.7) | 2 (2.7) | 0.685 | | Incidence of urethral stricture | 4 (5.4) | 5 (6.7) | 0.508 | | Post-operative IPSS | | | | | 3 months | 8.5±2.2 | 8.9±2.5 | 0.278 | | 6 months | 8.5±2.1 | 8.9±2.4 | 0.267 | | Post-operative Qmax, mL/s | | | | | 3 months | 19.0±3.1 | 18.7±3.3 | 0.576 | | 6 months | 19.2±3.2 | 18.9±3.3 | 0.581 |
|
|
Operative and post-operative characteristics.
|

|
|
Changes from baseline to 3 months and 6 months after surgery. (A) IPSS overall; (B) Qmax overall; (C) IPSS in the M-TURP group; (D) Qmax in the M-TURP group; (E) IPSS in the B-TURP group; (F) Qmax in the B-TURP group. IPSS, the International Prostate Symptom Score; Qmax, maximum urinary flow rate; Pre-op, pre-operative; CI, confidence interval; TURP, transurethral resection of prostate; B-TURP, bipolar TURP; M-TURP, monopolar TURP.
|
| Prostate size, mL | M-TURP (n=74) | p-Value | B-TURP (n=75) | p-Value | | n (%) | Operative time, median (range), min | n (%) | Operative time, median (range), min | | <40 | 12 (16.2) | 30 (20-40) | <0.001a | 9 (12.0) | 30 (25-30) | <0.001b | | 40-59 | 32 (43.2) | 40 (20-60) | 35 (46.7) | 35 (30-50) | | 60-99 | 25 (33.8) | 45 (25-60) | 30 (40.0) | 50 (30-70) | | ≥100 | 5 (6.8) | 70 (70-90) | 1 (1.3) | 50 |
|
|
Correlation of prostate size with operative time.
|
| Parameter | Univariate analysis | | HR | 95% CI | p-Value | | Prostate size, mL | 0.002 | (0.000, 0.004) | 0.04 | | Operative time, min | ?0.004 | (?0.007, 0.000) | 0.048 | | Grade of injury | | | | | Grade I | 0.148 | (0.028, 0.194) | 0.009 | | Grade II | 0.33 | (0.216, 0.443) | <0.001 | | Grade III | 1.015 | (0.849, 1.182) | <0.001 |
|
|
Covariates associated with stricture.
|
|
|
Grade injury wise occurrence of SU. SU, stricture urethra.
|
| Parameter | Stricture | p-Value | | Yes (n=9) | No (n=140) | | Prostate size, mL | 65.0 (35.0-150.0) | 50.0 (25.0-143.0) | 0.03 | | Hypertension or diabetes | 3 (33.3) | 16 (11.4) | 0.09 | | Operative time, min | 55.0 (30.0-70.0) | 40.0 (20.0-90.0) | 0.002 | | Incidence of urethral rupture | 9 (100.0) | 21 (15.0) | <0.001 | | Grade of injury | | | | | Grade I | 2 (22.2) | 15 (10.7) | 0.273 | | Grade II | 3 (33.3) | 6 (4.3) | 0.011 | | Grade III | 4 (44.4) | 0 | <0.001 |
|
|
Correlation of various parameters with stricture.
|
| [1] |
Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol 2004 ; 46:547-54.
|
| [2] |
Mamoulakis C, Trompetter M, de La Rosette J. Bipolar transurethral resection of the prostate: the “golden standard” reclaims its leading position. Curr Opin Urol 2009; 19:26-32.
|
| [3] |
Michielsen DP, Coomans D, Engels B, Braeckman JG. Bipolar versus monopolar technique for palliative transurethral prostate resection. Arch Med Sci 2010; 6:780-6.
|
| [4] |
Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)dincidence, management, and prevention. Eur Urol 2006; 50:969-79.
|
| [5] |
Tan GH, Shah SA, Ali NM, Goh EH, Singam P, Ho CCK, et al. Urethral strictures after bipolar transurethral resection of prostate may be linked to slow resection rate. Investig Clin Urol 2017; 58:186-91.
|
| [6] |
Issa MM. Technological advances in transurethral resection of the prostate: bipolar versus monopolarturp. J Endourol 2008; 22:1587-95.
|
| [7] |
Doluoglu OG, Gokkaya CS, Aktas BK, Oztekin CV, Bulut S, Memis A, et al. Impact of asymptomatic prostatitis on re- operations due to urethral stricture or bladder neck contracture developed after TUR-P. Int Urol Nephrol 2012; 44:1085-90.
|
| [8] |
Michielsen DP, Coomans D. Urethral strictures and bipolartrans urethral resection in saline of the prostate: fact or fiction? J Endourol 2010; 24:1333-7.
|
| [9] |
Eri LM, Thomassen H, Brennhovd B, Ha°heim LL. Accuracy and repeatability of prostate volume measurements by transrectal ultrasound. Prostate Cancer Prostatic Dis 2002; 5:273-8.
|
| [10] |
Reich O, Gratzke C, Stief CG. Techniques and long-term results of surgical procedures for BPH. Eur Urol 2006; 49:970-8.
|
| [11] |
Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. Eur Urol 2009; 56:798-809.
|
| [12] |
Sciarra A, Salciccia S, Albanesi L, Cardi A, D’Eramo G, Di Silverio F. Use of cyclooxygenase-2 inhibitor for prevention of urethral strictures secondary to transurethral resection of the prostate. Urology 2005; 66:1218-22.
|
| [13] |
Park JK, Lee SK, Han SH, Kim SD, Choi KS, Kim MK. Is warm temperature necessary to prevent urethral stricture in combined transurethral resection and vaporization of prostate? Urology 2009; 74:125-9.
|
| [14] |
Villaa P, Ugaldea MS, Martínb ML, Pe?a FM. Risk factors for developing urethral stricture in patients that underwent transurethral resection of the prostate. Rev Mex Urol 2013; 73:166-74.
|
| [15] |
Hoffmann R. [Transurethrale resektion (TURP) und transurethrale inzision (TUIP) der prostata]. In: HoffmannR, editor. EndoskopischeUrologie. Heidelberg: Springer; 2005. p. 50-84. [Book in German].
|
| [16] |
Lentz HC Jr, Mebust WK, Foret JD, Melchior J. Urethral strictures following transurethral prostatectomy: review of 2223 resections. J Urol 1977; 117:194-6.
|
| [17] |
Varkarakis J, Bartsch G, Horninger W. Long-term morbidity and mortality of transurethral prostatectomy: a 10-year follow-up. Prostate 2004; 58:248-51.
|
| [18] |
Wang JW, Man LB. Transurethral resection of the prostate stricture management. Asian J Androl 2020; 22:140-4.
|
| [19] |
Mundy AR, Andrich DE. Urethral strictures. BJU Int 2011; 107:6-26.
|
| [20] |
Komura K, Inamoto T, Takai T, Uchimoto T, Saito K, Tanda N, et al. Incidence of urethral stricture after bipolar transurethral resection of the prostate using TURis: results from a randomized trial. BJU Int 2015; 115:644-52.
|
| [21] |
Smith TG. Current management of urethral stricture disease. Indian J Urol 2016; 32:27-33.
|
| [22] |
Sarier M, Duman I, Kilic S, Yuksel Y, Demir M, Aslan M, et al. Comparative results of transurethral incision with transurethral resection of the prostate in renal transplant recipients with benign prostate hyperplasia. Urol J 2018; 15:209-13.
|
| [23] |
Sarier M, Duman I, Demir M, Yuksel Y, Emek M, Kukul E. The outcomes of transurethral incision/resection of the prostate (TUIP/TURP) performed early after renal transplantation. Turk Uroloji Dergisi/Turkish. J Urol 2018; 44:172-7.
|
| [24] |
Kulkarni SB, Joglekar O, Alkandari M, Joshi PM. Management of post TURP strictures. World J Urol 2019; 37:589-94.
|
| [1] |
Noura F. Abbas, Marc R. Aoude, Hampig R. Kourie, Humaid O. Al-Shamsi. Uncovering the epidemiology of bladder cancer in the Arab world: A review of risk factors, molecular mechanisms, and clinical features[J]. Asian Journal of Urology, 2024, 11(3): 406-422. |
| [2] |
Nikita Shrivastava, Rahul Jena, Deepak Prakash Bhirud, Mahendra Singh, Gautam Ram Choudhary, Arjun Singh Sandhu. Analysis of the urethral stricture score and patient-related factors as predictors of outcomes following oral mucosal graft urethroplasty[J]. Asian Journal of Urology, 2024, 11(3): 473-479. |
| [3] |
Ahmed M. Abdel Gawad, Abhijit Patil, Abhishek Singh, Arvind P. Ganpule, Ravindra B. Sabnis, Mahesh R. Desai. Long-term outcomes of urethral balloon dilation for anterior urethral stricture: A prospective cohort study[J]. Asian Journal of Urology, 2024, 11(3): 480-485. |
| [4] |
Gede W.K. Duarsa, Yeremia G. Kusumah, Ronald Sugianto, Pande M.W. Tirtayasa, Tjokorda G.B. Mahadewa. Tumor necrosis factor-alpha, transforming growth factor-beta, degree of lower urinary tract symptoms as predictors of erectile dysfunction in benign prostatic hyperplasia patients[J]. Asian Journal of Urology, 2024, 11(2): 280-285. |
| [5] |
U Phun Loo, Chun Hou Yong, Guan Chou Teh. Predictive factors for percutaneous nephrolithotomy bleeding risks[J]. Asian Journal of Urology, 2024, 11(1): 105-109. |
| [6] |
Pankaj M. Joshi, Manuel Hevia, Yatam Lakshmi Sreeranga, Marco Bandini, Amey Patil, Shreyas Bhadranavar, Vipin Sharma, Sandeep Bafna, Sanjay B. Kulkarni. Double-face urethroplasty in patients with obliterative bulbar strictures post-transurethral resection of the prostate mid-term outcomes in high-volume referral center[J]. Asian Journal of Urology, 2023, 10(4): 512-517. |
| [7] |
Tsung Mou, Oluwateniola Brown, Yingxiao Hua, Melissa Simon, XinQi Dong, Kimberly Kenton, C. Emi Bretschneider. Gender differences of lower urinary tract symptoms in older Chinese Americans[J]. Asian Journal of Urology, 2023, 10(4): 526-533. |
| [8] |
Zhao Wang, Kaixuan Li, Quan Zhu, Haozhen Li, Ziqiang Wu, Xuesong Liu, Zhengyan Tang. Incidence and risk factors of in-hospital venous thromboembolism in non-oncological urological inpatients: A single center experience[J]. Asian Journal of Urology, 2023, 10(4): 546-554. |
| [9] |
Xiaowei Yang,Lynn Sayer,Sam Bassett,Sue Woodward. The prevalence, associated factors, and impact of urinary incontinence in pregnant and postpartum women in Nanjing, China: A cross-sectional study[J]. Asian Journal of Urology, 2023, 10(3): 337-343. |
| [10] |
Rajiv N. Kore. Management of urethral strictures and stenosis caused by the endo-urological treatment of benign prostatic hyperplasia—a single-center experience[J]. Asian Journal of Urology, 2023, 10(2): 137-143. |
| [11] |
Mohammad Shazib Faridi,Vikas Sharma,Adittya K. Sharma,Rahul Yadav. Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture: A prospective randomised pilot study[J]. Asian Journal of Urology, 2023, 10(2): 189-194. |
| [12] |
Maryam Emami,Pejman Shadpour,Koosha Kamali,Nima Narimani,Jalil Hosseini. Female anterior wall onlay urethroplasty with lower lip buccal mucosal graft: Importance of the laterally extended incision[J]. Asian Journal of Urology, 2023, 10(1): 33-38. |
| [13] |
Yudhistira Pradnyan Kloping,Niwanda Yogiswara,Yusuf Azmi. The role of preoperative dutasteride in reducing bleeding during transurethral resection of the prostate: A systematic review and meta-analysis of randomized controlled trials[J]. Asian Journal of Urology, 2022, 9(1): 18-26. |
| [14] |
Alberto Abrate,Andrea Gregori,Alchiede Simonato. Lingual mucosal graft urethroplasty 12 years later: Systematic review and meta-analysis[J]. Asian Journal of Urology, 2019, 6(3): 230-241. |
| [15] |
Liu Yu,Chen Yuntian,Liao Banghua,Luo Deyi,Wang Kunjie,Li Hong,Zeng Guohua. Epidemiology of urolithiasis in Asia[J]. Asian Journal of Urology, 2018, 5(4): 205-214. |
|
|
|
|